Last month, we covered “route-specific” ADE/PDE values as a possible basis for cleaning validation limits. This month, we will cover the issue of duration of exposure for setting ADE/PDE values. In other words, if the product containing a carryover residue was to be only administered for a short time (not a lifetime), is it possible to be less stringent in setting limits? Just to clarify, I am discussing this even though ISPE’s Risk-MaPP defines ADE as a safe value for a lifetime exposure, and even though the EMA “dedicated” guidance defines PDE as for a lifetime exposure. However, I should clearly state that even though there is a section in the EMA document dealing with Investigational Medicinal Products, there is no mention in that document of adjustments based on the duration of patient exposure. Furthermore, Risk-MaPP also does not address the issue of shorter exposures except for application of the TTC concept to genotoxic materials in a manner similar to ICH M7 (keep reading).
So, why am I bringing this up? Well, ICH M7 (“Assessment and Control of DNA Reactive (Mutagenic) Impurities in Pharmaceuticals to Limit Potential Carcinogenic Risk”) focuses on the TTC (Threshold of Toxicological Concern) concept (which is presented by the EMA as an alternative “safe threshold value”). M7 states that “established cancer risk assessments are based on lifetime exposures”, but that “Less-Than-Lifetime (LTL) exposures both during development and marketing can have higher acceptable intakes of impurities and still maintain comparable risk levels.” How does M7 present this possibility?
Well, it gives the standard 1.5 µg/day as an acceptable value for any mutagenic impurity for a lifetime exposure (lifetime being greater than 10 years). Section 7.3 of M7 covers “Acceptable Intakes in Relation to LTL Exposure”. Based on the assertion that “cancer risk of a continuous low dose over a lifetime would be equivalent to the cancer risk associated with an identical cumulative exposure averaged over a shorter duration”, TTC values are presented in Table 2 in M7 for LTL exposures as follows:
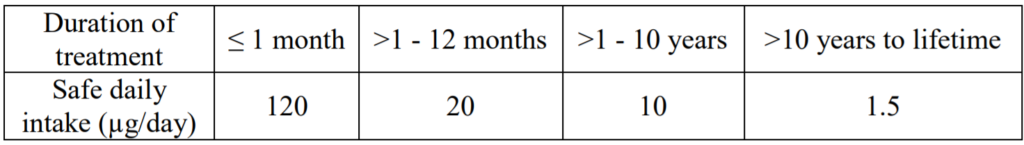
Note: I have added the term “Safe” to the daily intake description in the table above; it is a reasonable assumption that that term is implied.
Before I get to discussing cleaning validation residues and limits, let me make it clear that I highly recommend you carefully read ICH M7 before making any decisions on limits for mutagenic impurities. My only reason for bringing it up is that it allows for duration-specific limits. And my question is whether an analogous approach could be used for cleaning validation residue limits.
I should also emphasize that M7 applies to impurities in drug actives and therefore in drug products. Many will interpret the issue of “impurities” as a manufacturing impurity, meaning an impurity present as a result of a chemical synthesis or subsequent degradation of the active. Such a view would exclude a cleaning process residue as being considered an impurity under M7 and other ICH guidelines such as Q3C. In one sense, what difference does it make what the source of the impurity is? Shouldn’t what is acceptable for a manufacturing impurity also apply to a cleaning residue impurity?
However, as a practical matter, cleaning validation residues have generally been held to a more stringent standard than manufacturing impurities. Part of the reason is that a major focus of cleaning validation residues has been drug actives, which are known to have a pharmacological effect. Information on the safety/toxicity of manufacturing impurities may be less specific. The only situation where a good case can be made for treating manufacturing impurities and cleaning validation residues the same is for mutagenic species; in that case, the potential harm might be the same.
Please treat these last two paragraphs as a side issue to what I am really getting at, which is the possibility of setting cleaning validation limits less stringently for short-term possible exposure situations, such as for materials made in a clinical setting. Using the same ratio given in Table 2 in M7, could we set limits higher by a factor of about 100 for situations where the drug product will be taken only up to one month? Or, can we set cleaning validation limits higher by a factor of about 13 if exposure is no more than 12 months? Remember also that the duration of exposure is not that of the cleaned product, but rather of the next product manufactured in that cleaned equipment. Determining and/or controlling the duration of that exposure may be problematic.
If we take a look at a setting where I am making only clinical trial materials, the strategy of making limits higher because of the limited duration of exposure is probably not one that I would recommend. The reason is that, as a company taking a product to clinicals, I would prefer that the drug product be representative of what I could produce on a commercial scale (so that my clinical trial results would be predictive of patient results when I went commercial). Having a significantly different residue profile for a product for a clinical trial is problematic. We should also remember that if I set higher limits for the cleaning of my product, it is the next product manufactured (not necessarily my product) that is affected.
The situation for a commercial product is slightly different. Let’s say I only manufacture antibiotics on certain equipment. If those antibiotics are only given for a short duration (less than 2 weeks, for example), is it possible to set my PDE/ADE values 100 times higher (about the same ratio used in Table 2 of M7) as compared to a safe level for a lifetime exposure? That certainly is a possibility, but look at the likely effect. At that level, I might be allowing about 10% of a daily dose up to a full daily dose of that antibiotic in the next manufactured antibiotic. Clearly that would be an unacceptable situation. Particularly as firms move away from a 0.001 dose criterion to an ADE/PDE criterion, that approach should be avoided (Note: I would also tend to avoid such a dramatic adjustment even based on a dose criterion).
What if I am manufacturing both products with short duration frequencies and those with long duration frequencies on the same equipment (such as manufacturing both commercial products and clinical trial materials on the same commercial equipment)? The possibilities become so complex that it becomes impractical to say limits can be less stringent. Further, my earlier point about the quality of the clinical material being similar to the quality of commercial material (if the clinical product becomes commercial) also applies.
I would also tend to discourage firms from setting less stringent limits based on the expectation that those less stringent limits would result in visually soiled equipment, as well as potentially affecting other quality parameters of the next product, including efficacy, stability, and purity.
So, my emphasis for this situation (duration-based limits) is different from what I presented last month (for route-specific limits). The major difference is that route-specificity is something that I can control adequately (all products in this facility/equipment are administered by the oral route). Duration specificity is something harder to control; my expectation is that trying to implement and consistently control such a program would be difficult in many situations. So, unless you are in a situation where duration of product exposure is well-controlled, there are probably ways to improve efficiency other than setting limits less stringently based on duration of exposure of the subsequently manufactured product.